A Service Design Perspective on the Rollout of New Federal Disability Funding
Service design is playing an ever increasing role in large systemic changes in which there are human elements. A systemic, service design approach could support the roll out of the NDIS (National Disability Insurance Scheme) for individuals with mental health needs. It is critical to ensuring that the needs of individuals with mental disabilities, carers of the individuals and providers of mental health disability services are met, that they all transition well through this process and equally benefit from the changes.
At Meld we’re incredibly proud to work with a number of organisations who work in and around health and wellbeing in Australia. A good deal of my own design career has been spent considering how to design for outcomes in health and wellbeing, having worked in a medical devices team in New Zealand, and on many preventative initiatives for health and wellbeing with the New Zealand government in Wellington.
In May I attended the VICSERV Mental Health Conference with the intent of understanding the mental health paradigm in Australia. Having recently come from New Zealand, I wanted to understand what organisations in Australia are doing to support the carers and consumers of Mental Health services. The conference centred around 3 themes: Hope, Innovation and Co-design - 3 themes that reverberate strongly in the design world, in particular at Meld Studios.
Sitting in the first sessions of the conference it became clear that I had walked into a frustrated community who were experiencing a major shift in the way the they were going to be approaching the delivery of their services in the future. That shift is called the National Disability Insurance Scheme or NDIS.
A quick look at the NDIS website tells us that:
"The NDIS supports people with a permanent and significant disability that affects their ability to take part in everyday activities.
We will work with you to identify supports you need to live your life. Supports may help you achieve goals in many aspects of your life, including independence, involvement in your community, education, employment and health and wellbeing.
The NDIS gives you more choice and control over how, when and where your supports are provided, and gives you certainty you will receive the support you need over your lifetime."
The NDIS was something I was completely oblivious to before attending the conference. So like any designer who has an optimistic dissatisfaction for people's experiences within complex systems and who has a penchant for undercover research would do - I decided to talk to the people on the ground. This took place at the conference, in between scoffing tuna wraps during the breaks.
The following is an account of some of the important things I heard and how a service design approach relates.
(Quotes are paraphrased from about 20 conversations over the two days as to not identify any individual or organisation.)
Providers aren’t sure what it all means
It’s there, it’s done and being implemented gradually. We still don’t know what the full effects will be really.. There’s not a single source of the truth
It's believed that what the system defines as "disabled" in regards to mental health will change. There will be people with a mental illness which was once considered disabling, and won't be under this new system. Those people will start to lose out.
There is an interesting thing when people make decisions on the behalf of others. It's not something we can avoid, as we have people make decisions on our behalf all the time, but often what happens is everyone understands needs in a different way. What we try to do is to create a shared understanding - this is done by being purposeful in doing so, having an inclusive and participatory process and great communication design.
Shifting from block to individualised, needs-based funding
The shift, as I mentioned earlier, for an organisation and the community was summed up excellently by one attendee as:
A community of organisations who once had to work together due to limited resources, are now going to be made to compete for those same limited resources on an open market.
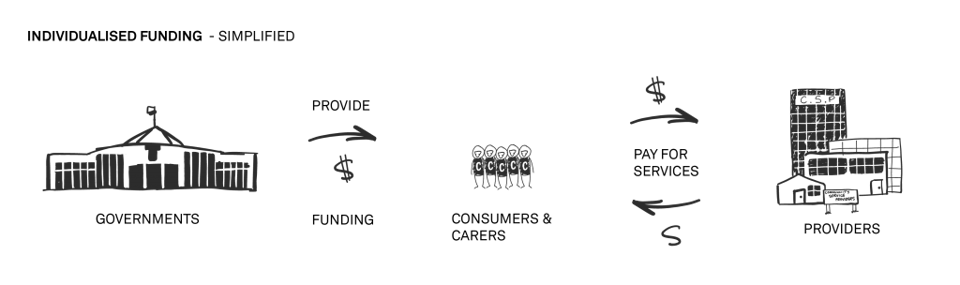
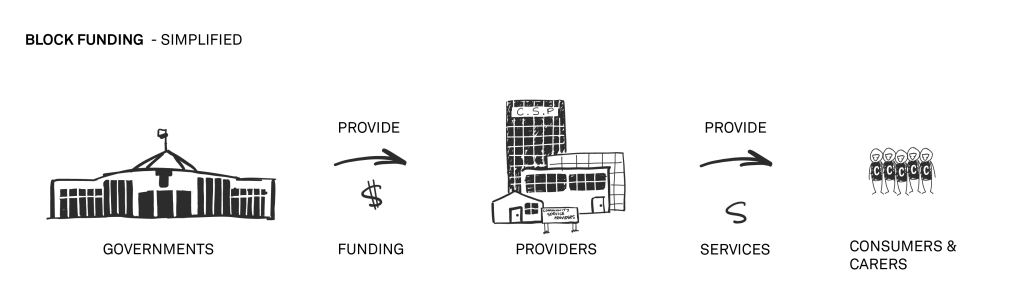
What this means is with the introduction of the NDIS disability support is moving toward individualised funding based on individualised needs assessment, and away from block funding.
What this could mean, if we don’t pay close enough attention, is that consumers of mental health services may have an increase in control, but it may be at the expense of the number choices. This is the heart of the issue in the roll out. The organisations who have provided care for decades, who have the right history and the skilled employees are now faced with a new reality, and it's possible that some may not survive it.
What happens when we change big, complex things?
Shifting toward needs-based, individualised funding within welfare systems has great benefits. However, the network of community service providers at the conference have been built, over decades, to work in a very different system. Those who provide support aren't structured or setup to exist in a system where they are competing with others. Much like the unforeseen consequences of deinstitutionalisation, making a change without explicit understanding of the interconnectedness which defines the system may likely lead to enormous repercussions.
This raises a range of questions about changing large systems - mostly around the importance of understanding interconnectedness before attempting to change it as a whole.
We need to be thinking about what happens to those organisations who fail to adapt within this new funding framework. Is it ethical for the government to make fundamental changes to a system which businesses rely on it to exist? Should the government have helped design a transition? Who’s responsible for giving support to help small organisations reorient and develop new business and operation models? How do they afford to adapt? How do we make sure skilled and compassionate people with the right experience don't lose their jobs or businesses? How does the community care sector avoid falling away, and adapt to changes of the this kind of shift?
Simply put: How do these organisations begin to move forward from today?
How might organisations reorient themselves for a new system?
There were a few things being done by organisations and individuals from the conference who are starting to make changes. I’ll look to examine these in relation to service design methods:
Identifying emerging challenges is the first step in making meaningful change.
One problem is that we’re now expecting only to be paid for face-time. We’re serving a lot of rural consumers and part of that service is needing to travel to them. If you’re driving 2 hours for a round trip we might not get paid for that. We do now, but we’re not sure under NDIS. This could mean, if we don’t get creative enough with how we deliver those services, rural consumers might not have as many options.
Service design gives us the ability to qualitatively identify challenges and their interconnections, which then gives us the chance to reframe those challenges as opportunities to change for the better.
Looking outside of your current value proposition in order to see your assets in a new light can be a “creative” way to approach change.
We’re having to broaden our service offering to include non-mental health services. That’s in order to fund services that were previously wholly covered with the previous scheme. We’re stretched as a result.
Service design helps us to understand the value that is possible and compatible with your business by understanding what the people inside and outside of your organisation value.
It’s about the experience, as well as the care you provide
We know organisations don't really compete on price these days. They barely complete on what they can achieve either. World class organisations compete on the experience someone has with that organisation, and what it meant or means to them.
In challenging times, like this shift, the need for experience-led reorientation is even more important. The experiences staff and consumers have with an organisation can be the difference between it existing in future or not. The difference between A and B when the offer is the same. Understanding those current human experiences is the first step in times of transformation.
The short version
Service design does these things for organisations in times of transformation:
- Builds the understanding of your consumers and staff experiences, including their needs, desires and values
- Identifies challenges in meaningful contexts
- Reframes those challenges as opportunities to improve
- Shows interconnections, levers, and assets in the frame of ‘challenges as opportunities’
- Applies qualitative understanding to making decisions about opportunities
Please note: This post is not intended to answer questions about how to best provide care. It’s about shining a light on a challenge faced by many organisations in many industries and to explore the tools and mindset of service design in the task of business and sector transformation.
The problem of how to best provide care is also a complex and systemic one. As explored in Medibank’s report The case for Mental Health Reform in Australia (2013): “Fragmentation and insufficient coordination contribute to Australia’s sub-optimal mental health outcomes", something which the NDIS rollout may contribute to or go against, depending on how we approach it.
If you’d like to know more about service design, or want to help us build our knowledge of the health and wellbeing sector, please get in touch.